Abstract : Diabetes is one of the classic risk factors frequently associated with critical limb ischemia (CLI). For diabetic patients with CLI, the distribution of their atherosclerotic disease is typically localized to the tibial and pedal vessels, especially for diabetic patients with ischemic foot wounds or ulcerations. With diabetes affecting the smaller, distal blood vessels down to the foot, arterial disease is often difficult to detect using routine, non-invasive diagnostic testing, including duplex ultrasound and resting ankle-brachial indices (ABIs), as these testing methods limit the evaluation of arterial flow up to the level of the ankle. However, angiography is a powerful diagnostic and treatment tool, enabling accurate detection of stenotic and occlusive disease below the ankle and down to the toes. Although uncommon and technically challenging, successful revascularization performed in the pedal plantar loop and the digital branches beyond this loop can ensure optimal wound-healing outcomes for CLI patients with non-healing distal wounds on the lower extremities. For this case study, we present a patient with type 2 diabetes mellitus who developed a non-healing right hallux plantar ulceration. Despite non-invasive testing being normal in the office, severe stenotic and occlusive disease was angiographically detected in the digital branches, beyond the pedal plantar loop, supplying the right hallux. We discuss the treatment approach taken to target the patient’s disease and analyze the significant benefits of revascularization beyond the pedal plantar loop, particularly its role in promoting effective wound healing while lowering the risk of amputation.
J CRIT LIMB ISCHEM 2021;1(4):E160-E167. Epub 2021 November 23.
Key words: amputation prevention, chronic wounds, diabetes, endovascular treatment, non-healing wounds, wound healing.
Introduction
There is a clear association between diabetes and the prevalence of peripheral artery disease (PAD). Within the United States alone, there are approximately 12 million individuals suffering from PAD, with nearly one-third of these patients being diagnosed diabetics.1 The arteriopathy in the diabetic population is predominantly in the distal tibial and inframalleolar vessels.2 Diabetic PAD patients, in the more severe stages of their disease, can develop critical limb ischemia (CLI), which may manifest as ischemic ulcerations or gangrenous wounds that can increase the risk of lower-extremity amputation.3
Although infrequent and technically challenging, there is a clinical significance to performing arterial intervention in the pedal plantar loop and digital branches, specifically for CLI patients with distal wounds on the feet and toes, in order to prevent lower-extremity amputations.4 In this report, we present the case of a diabetic patient with a non-healing hallux ulceration. Angiographic evaluation revealed stenotic and occlusive disease in the digital arterial branches supplying the hallux, for which we outline the treatment approach and discuss the beneficial outcomes of revascularization.
Case Description
The patient was a 57-year-old Caucasian male with a >20-year history of insulin-dependent type 2 diabetes mellitus accompanied by severe peripheral neuropathy and a prior history of slow-healing, diabetic foot ulcers. Additional past medical history was significant for hypertension, hyperlipidemia on statin therapy, prior transient ischemic attack in 2010, and human immunodeficiency virus. During evaluation of social history, the patient identified as a non-smoker, denying prior usage of tobacco.
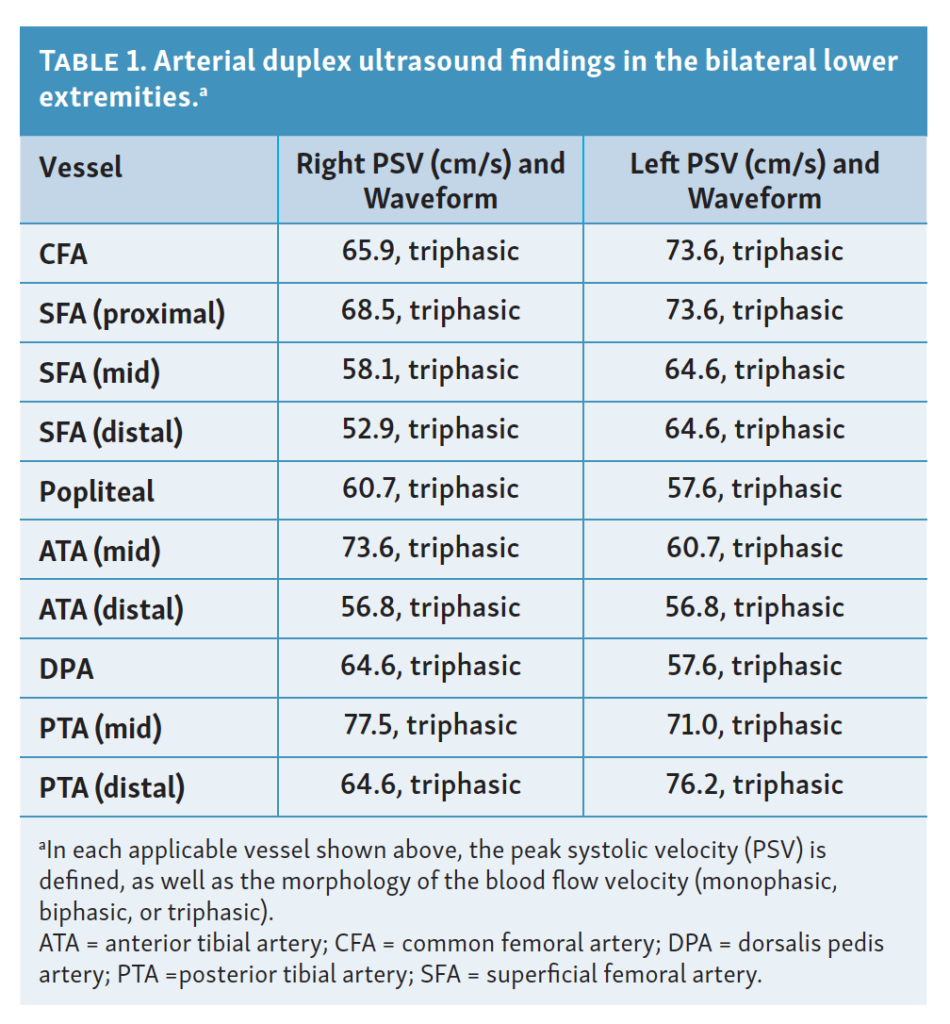
He presented to our clinic on December 23, 2020 for evaluation of an open, right hallux plantar ulceration (Figures 1A-1C) along with a “blister-like” ulceration to the base of the right, fifth digit (Figure 1D). The patient had been combating a current infection to the right hallux ulcer and was treated at the hospital with an irrigation and debridement procedure a few weeks prior, followed by administration of intravenous antibiotics.
In the clinic, the patient stated that both of the wounds on his right foot had been non-healing for the past 5-6 weeks. The etiology of these wounds was unknown to the patient, but he speculated that the wounds might have originated as shoe blisters. Since the inception of these digital ulcers, the patient’s wound care had been managed by his podiatrist, who referred the patient to our clinic for a vascular evaluation due to the patient’s impaired wound healing, prompting concern for compromised arterial flow in the foot.

The patient also complained of severe paresthesia to the bilateral feet, which was most prominent in the ulceration site of the right hallux. The patient stated that his podiatrist advised him to limit weight-bearing activities with the right foot, preventing him from keeping up with his activities of daily living. The patient also struggled with his balance and coordination on a daily basis due to the ulceration site at the right hallux. Upon further interview, the patient denied any prior revascularization procedures.
Physical examination revealed severe peripheral neuropathy with the patient scoring a 0/10 bilaterally on the Semmes-Weinstein monofilament test. There was loss of protective sensation from the mid tibia and downward, with the right lower extremity being worse than the left. Pedal pulses were easily palpable at the dorsum and the ankle bilaterally, scoring a 2+. Examination of the right foot demonstrated redness and non-pitting edema to the ulceration site at the right hallux and extending up the first metatarsal. The wound at the base of the right fifth digit was dry with eschar.
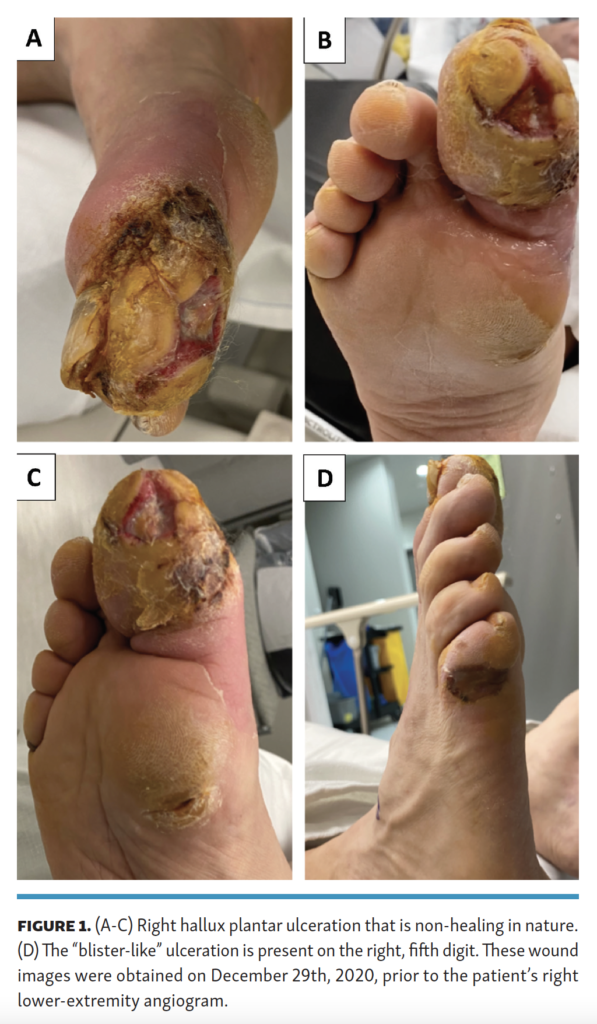
Diagnostic, non-invasive testing performed in the office was benign in nature, with the arterial duplex ultrasound revealing triphasic waveforms bilaterally (Table 1). No significant stenosis was detected via ultrasound in the bilateral femoropopliteal region, tibial arteries, and dorsalis pedis arteries (Table 1). The resting ankle-brachial indexes (ABIs) were 1.14 (right) and 1.60 (left). A toe-brachial index was not performed due to the right hallux ulceration.
In spite of the patient’s normal ultrasound and ABIs, given the chronic, non-healing nature of the wounds on the right foot along with the patient’s long-standing history of diabetes, a right lower-extremity angiogram with possible intervention was recommended. With diabetes being known to be associated with inframalleolar arterial disease, it was of utmost importance to proceed with angiographic evaluation due to the duplex ultrasound and ABIs limiting the vascular evaluation only up to the level of the ankle.
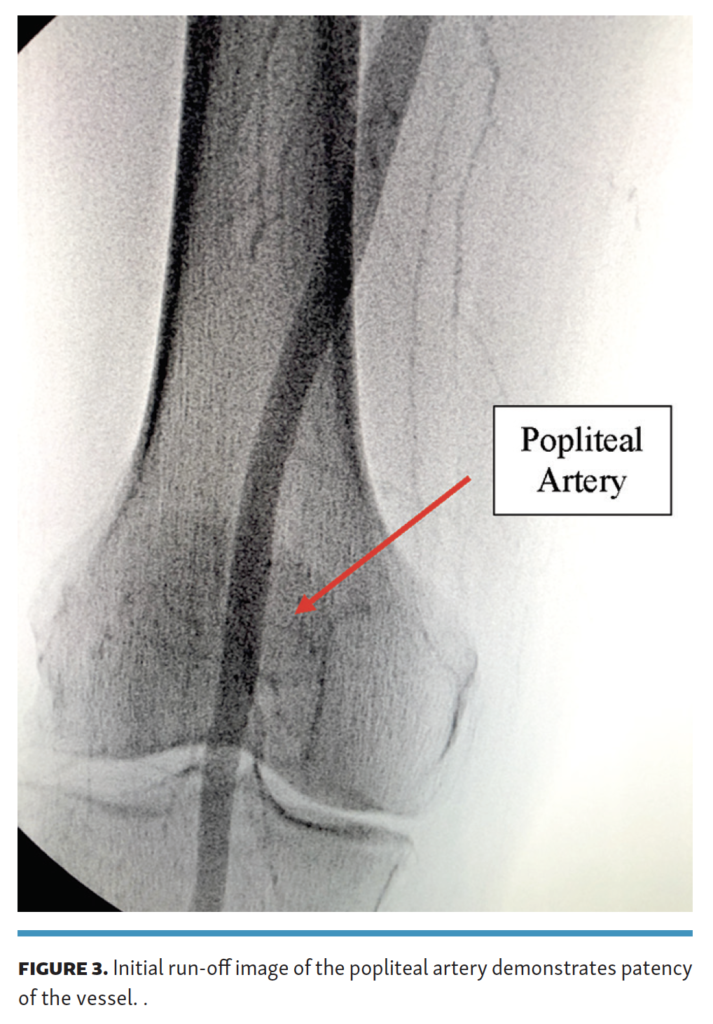
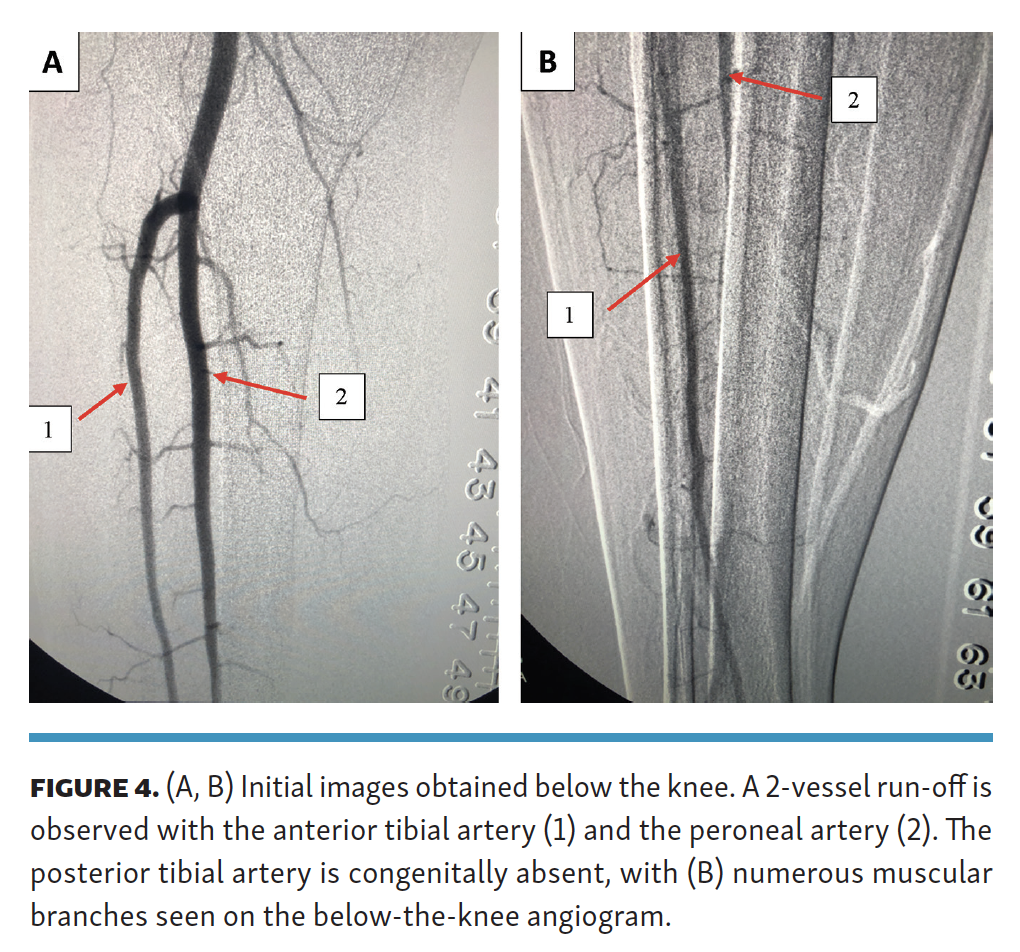
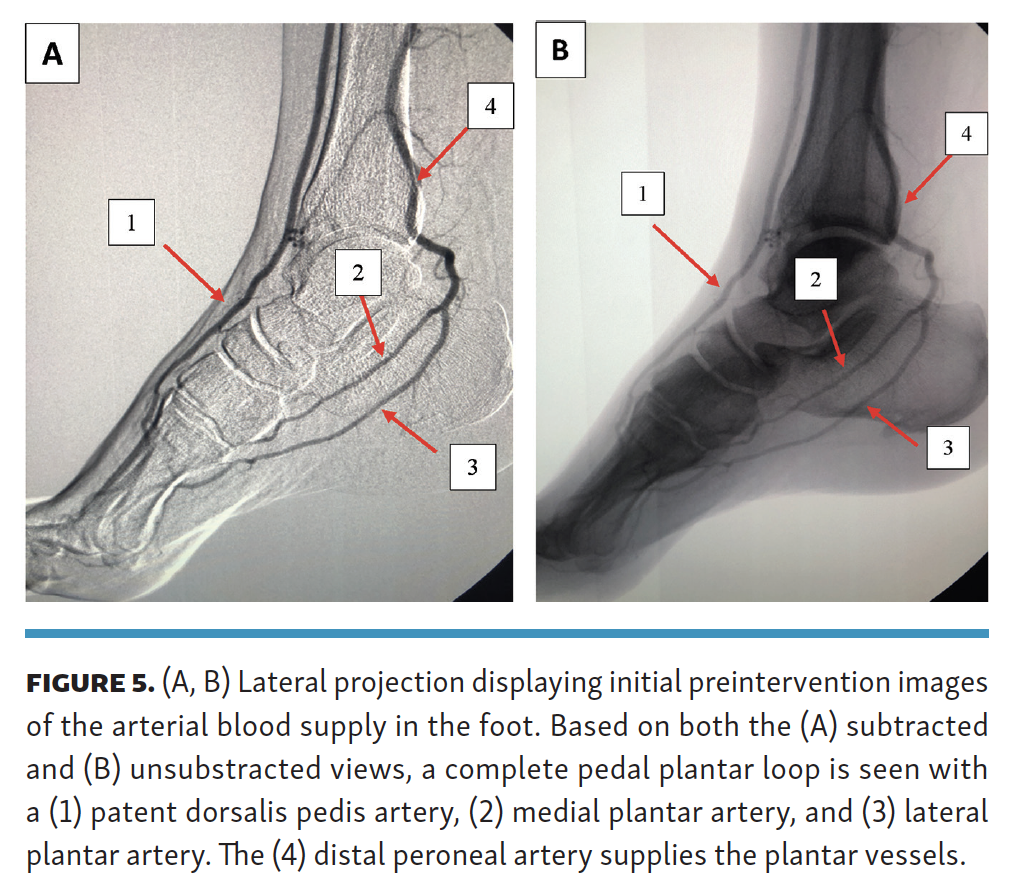
Approximately 1 week later, the patient presented to our office-based lab and a right lower-extremity angiogram was performed. Ultrasound-guided, antegrade access of the proximal superficial femoral artery was obtained since the patient’s aortoiliac inflow was patent, as indicated by his physical exam and duplex ultrasound findings (Figure 2A andTable 1). The initial angiographic run-off revealed no significant disease in the superficial femoral artery (Figures 2A, 2B) and popliteal artery (Figure 3), with a patent 2-vessel run-off involving the anterior tibial artery and the peroneal artery (Figures 4A, 4B). The patient’s posterior tibial artery was congenitally absent, with the peroneal artery continuing as the plantar vessels in the foot (Figures 5A, 5B). Pedal angiography revealed a patent dorsalis pedis artery, medial plantar artery, and lateral plantar artery, forming a complete pedal plantar loop (Figures 5A, 5B). At first glance, the angiographic findings seemed convincing enough to rule out a PAD diagnosis.
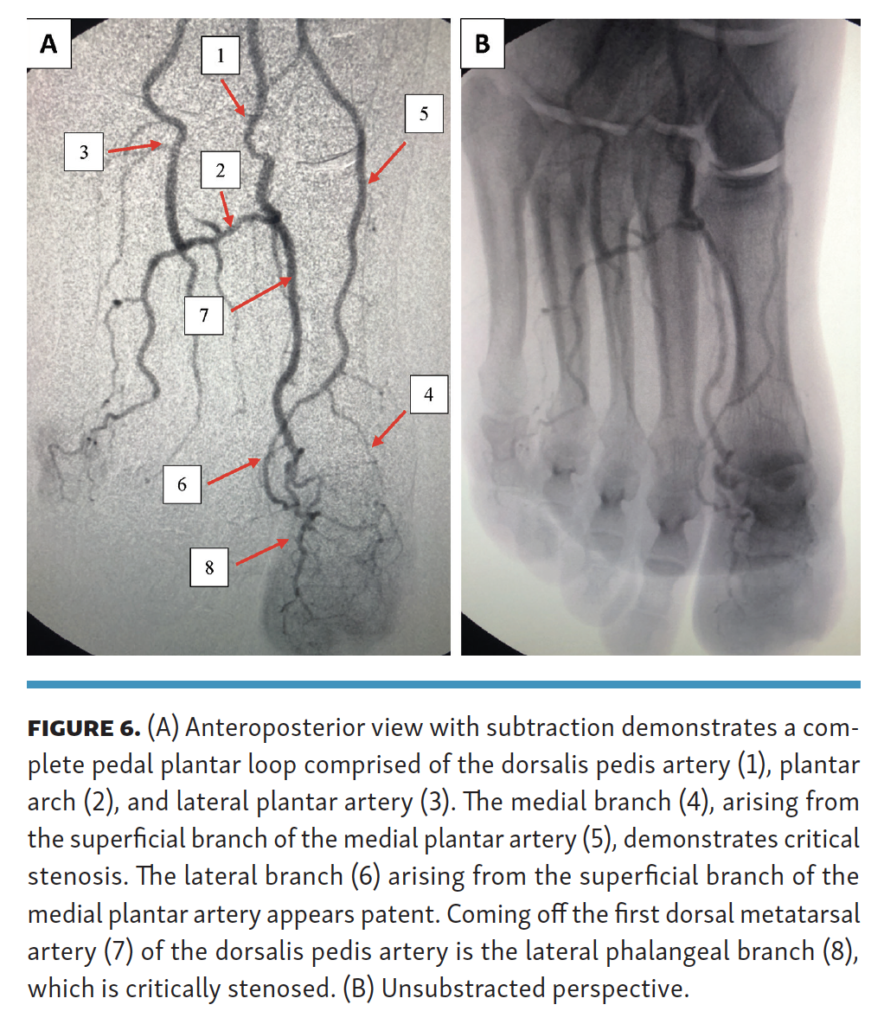
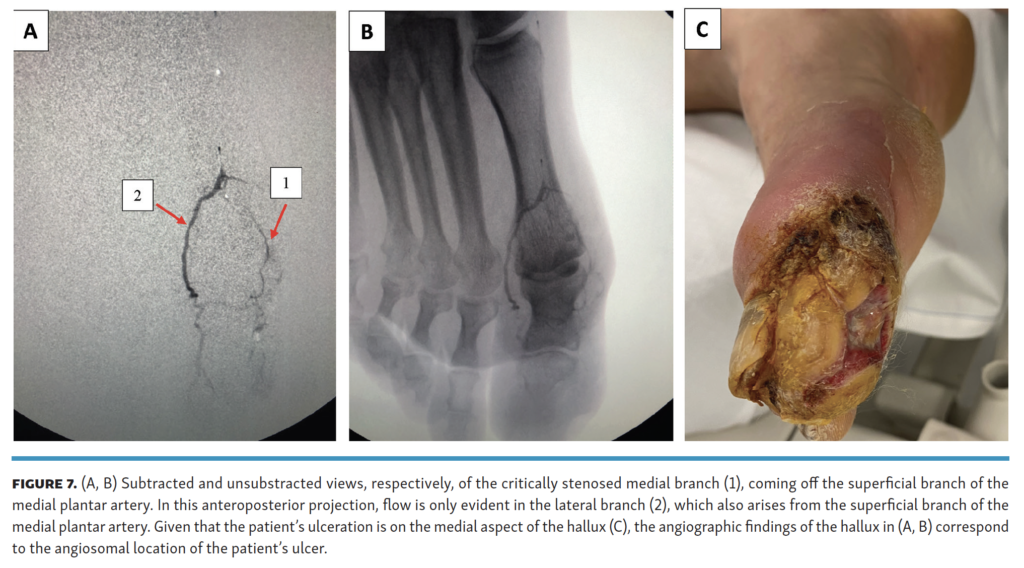

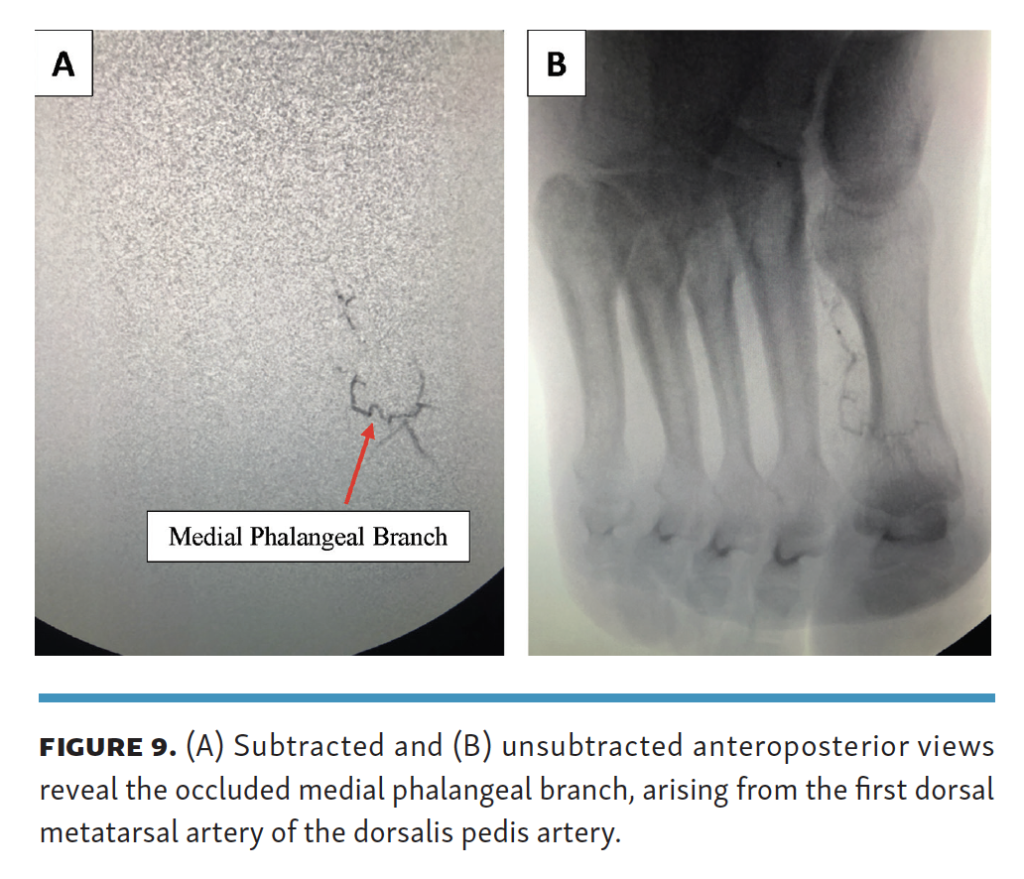
However, super-selective angiography beyond the pedal plantar loop demonstrated severe, critical stenosis involving the medial branch arising from the superficial branch of the medial plantar artery (Figures 6A, 6Band Figures 7A, 7B, 7C). Additional angiography demonstrated critical stenosis involving the distal aspect of the lateral phalangeal branch arising from the first dorsal metatarsal artery of the dorsalis pedis artery (Figures 6A, 6B and Figures 8A, 8B). The medial phalangeal branch coming off the first dorsal metatarsal artery of the dorsalis pedis artery was chronically occluded (Figures 9A, 9B).
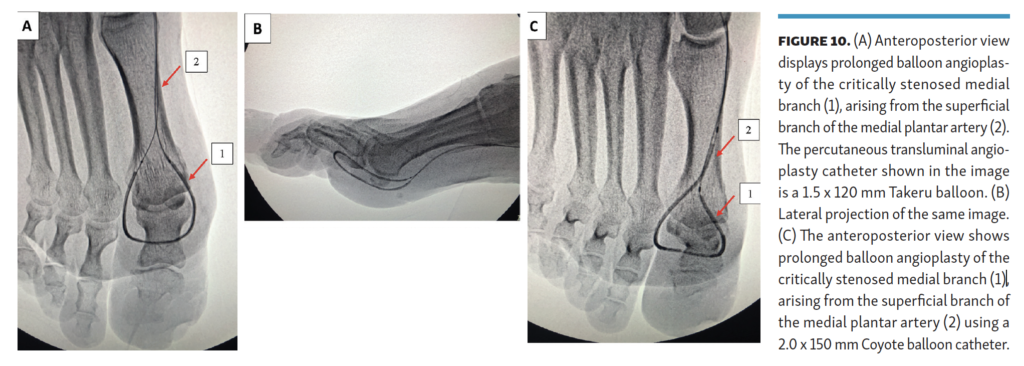
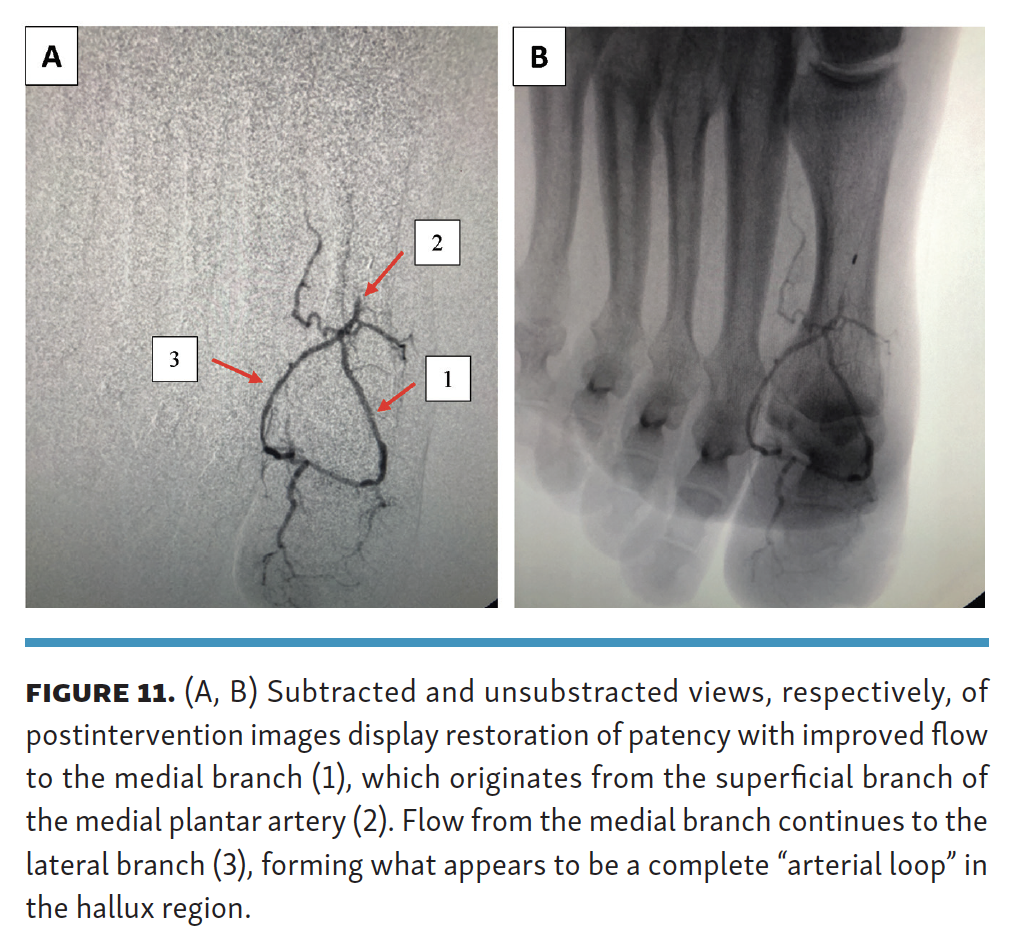
Following angiographic evaluation, the stenotic medial branch arising from the superficial branch of the medial plantar artery was successfully treated with percutaneous transluminal angioplasty using both a 1.5 x 120 mm Takeru balloon dilation catheter (Terumo) (Figures 10A, 10B) and a 2.0 x 150 mm Coyote balloon dilation catheter (Boston Scientific) (Figure 10C). Postangioplasty angiogram revealed good flow coming off the superficial branch of the medial plantar artery into the medial branch (Figures 11A, 11B). With restoration of patency to the medial branch, a complete “arterial loop” was angiographically observed in the region of the hallux, where there was continuous flow from the medial branch to the lateral branch, both arising from the superficial branch of the medial plantar artery (Figures 11A, 11B).
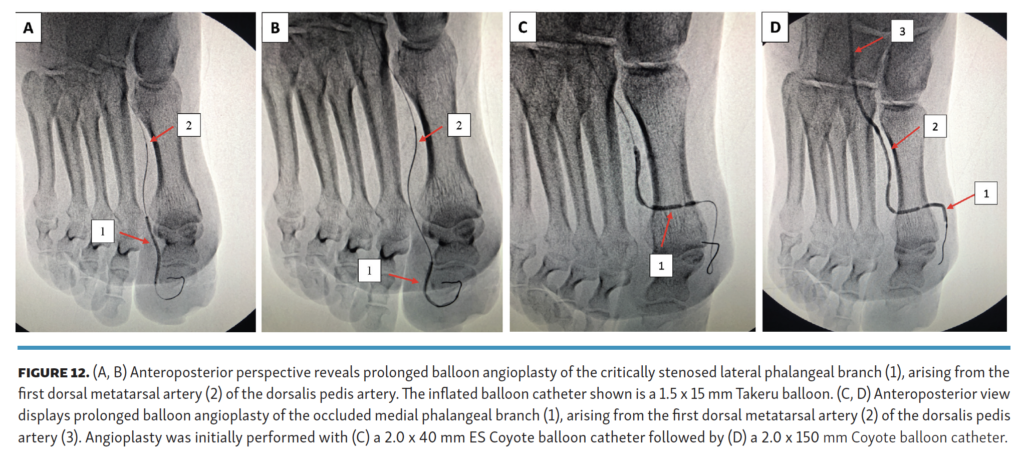
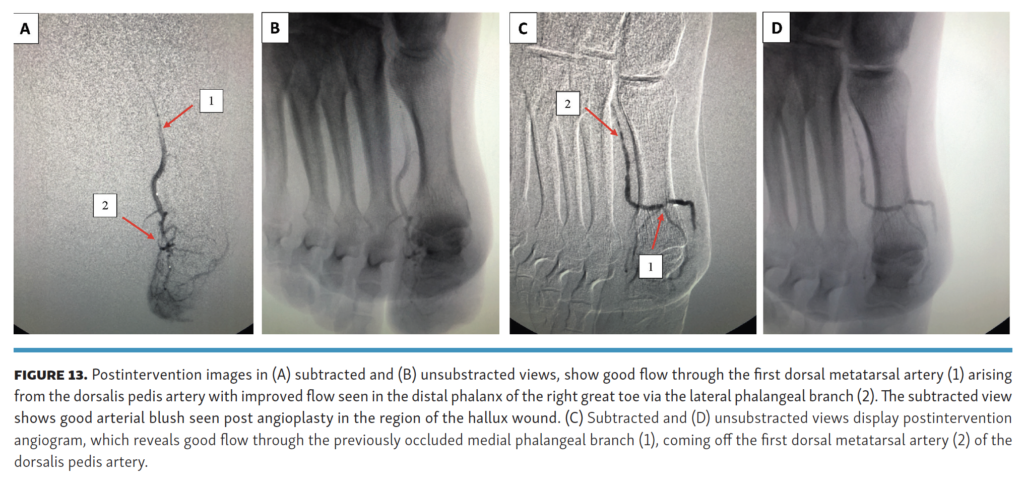
Prolonged balloon angioplasty was also performed on the critically stenosed lateral phalangeal branch coming off the first dorsal metatarsal artery from the dorsalis pedis artery, using a 1.5 x 15 mm Takeru balloon catheter (Figures 12A, 12B). The occluded medial phalangeal branch coming off the first dorsal metatarsal artery of the dorsalis pedis artery was successfully recanalized with a guidewire and angioplastied with a 2.0 x 40 mm Extra Support Coyote balloon catheter (Figure 12C), followed by a 2.0 x 150 mm Coyote balloon catheter (Figure 12D). The follow-up angiogram revealed significant improvement of flow into the distal phalanx of the right great toe (Figures 13A, 13B), including restoration of patency to the medial phalangeal branch, arising from the first dorsal metatarsal artery of the dorsalis pedis artery (Figures 13C, 13D). Postangioplasty angiogram further demonstrated good arterial blush within the region of the hallux wound (Figure 13A).
There was no peripheral sheath placed in the proximal SFA access site during the procedure. Instead, there was a 3 Fr inner dilator from the micropuncture kit inserted at the time of access, but all of the interventional balloons were bare backed. During the procedure, a total of 4000 units of heparin were administered intravenously. At the conclusion of the treatment, all wires and catheters were removed from the access site. Manual compression was held for approximately 5-6 minutes to achieve satisfactory hemostasis. Following the procedure, the patient was instructed to start dual-antiplatelet therapy, including acetylsalicylic acid 81 mg once daily for life and clopidogrel 75 mg once daily for 6 months.
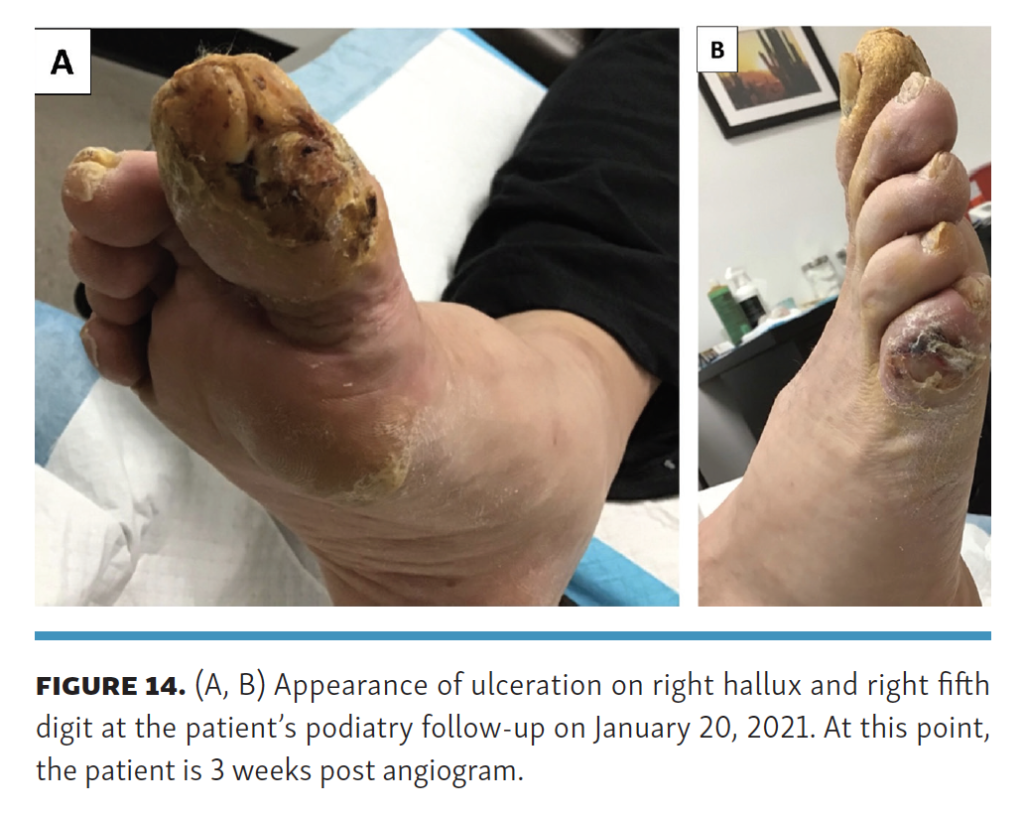
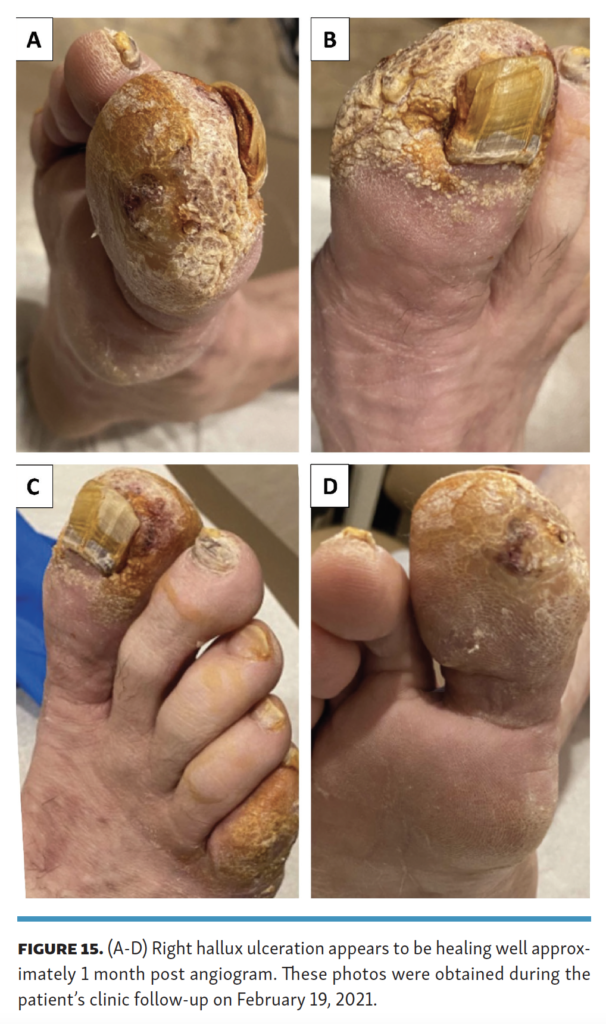
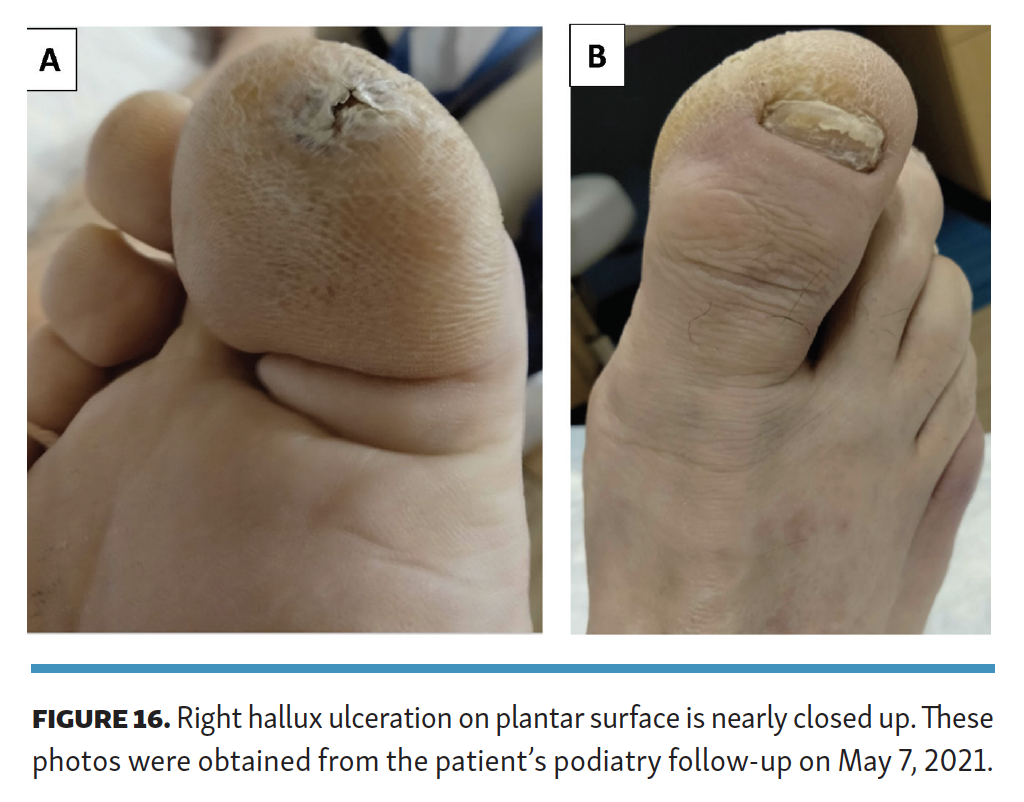
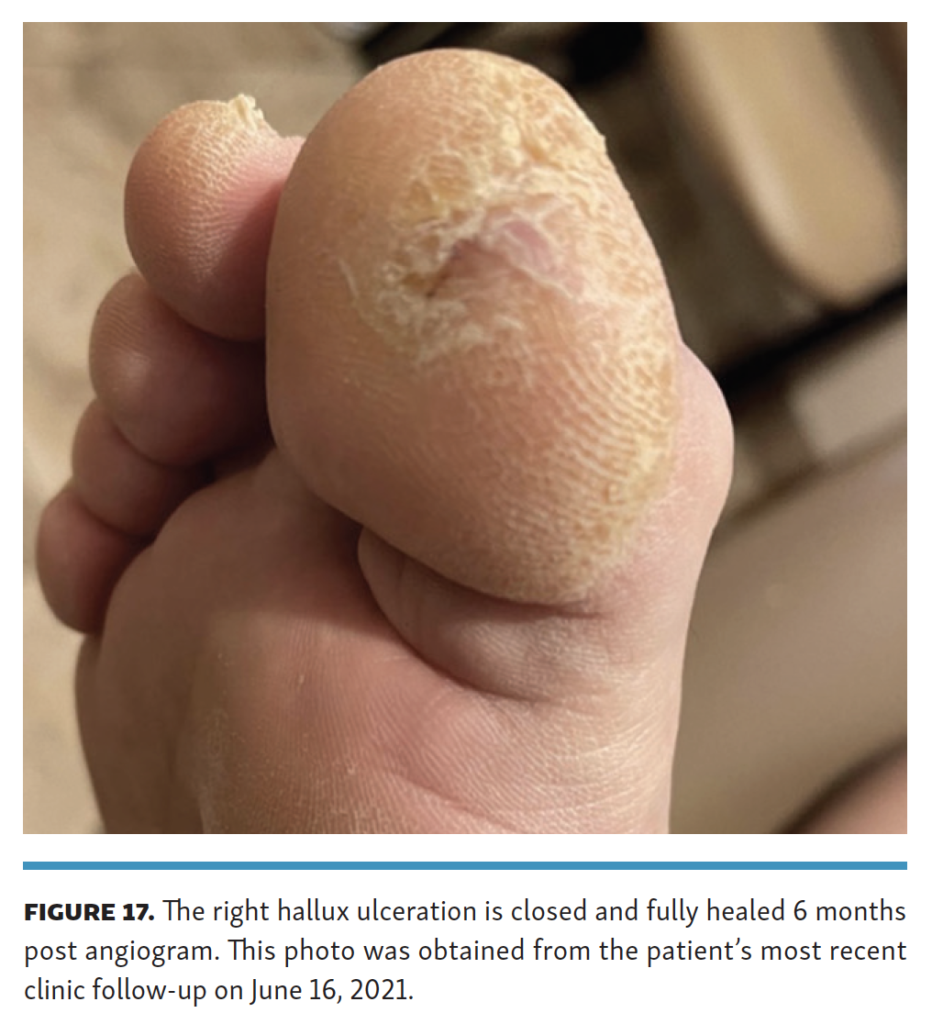
To track the progression of the wound-healing process, the patient was followed on a consistent basis by both our clinic and his podiatrist. With each monthly visit, the patient’s right foot wounds, particularly his right hallux ulceration, noticeably improved in appearance while decreasing in size (Figure 14, Figure 15, Figure 16). At 6-month follow-up angiogram, the patient’s right plantar hallux ulceration had fully healed (Figure 17). The “blister like” ulceration at the base of the right, fifth digit healed more quickly than the right hallux ulceration status post angiogram.’
Discussion
In many aspects, this case study illustrates that the screening and physical exam findings can be deceptively misleading when performing vascular evaluations in the office. In the case of this patient, he had normal duplex ultrasound findings, normal ABIs, and strongly palpable pedal pulses. However, if diagnostic testing and exam findings were prioritized over our own clinical suspicion, this patient would have been susceptible to digital amputation due to the non-healing nature of his right hallux ulceration. Indeed, this case study proves why it is essential to heavily interrogate and evaluate the patient’s clinical status and risk factors, as these components can help to piece together the justification required to proceed with an angiogram. This clinical mindset is especially relevant for diabetic patients, who can be difficult to evaluate clinically for PAD and CLI, considering that the presence of severe peripheral neuropathy can diminish the sensation of claudication, ischemic rest pain, or pain associated from diabetic foot ulcers or wounds.
Angiography serves as a very effective and essential diagnostic and treatment tool for CLI patients, especially those with non-healing wounds to the lower extremities. It is well established within the literature that successful revascularization of the pedal plantar loop through endovascular means can result in complete wound healing and a “higher rate of freedom from major amputation.”5,6 However, for this patient, despite his pedal plantar loop being complete during the initial run-off angiogram (Figures 5A, 5B), his hallux ulceration would not have successfully healed due to his disease residing beyond the pedal plantar loop.
To further aid this discussion, it is helpful to reference Taylor and Palmer’s classic angiosome concept (1987) to detail how successful wound healing was achieved for the patient through the intervention being performed on specific target arteries beyond the pedal plantar loop.7 The angiosome concept divides the foot and ankle region into 6 distinct vascular territories or “angiosomes” supplied by 3 main arteries, ie, the anterior tibial artery, peroneal artery, and posterior tibial artery.7 The anterior tibial artery transitions into the dorsalis pedis artery, while flow from the posterior tibial artery splits off into the calcaneal branch, medial plantar artery, and lateral plantar artery.7 Of particular interest to this case study, the hallux is categorized as an “independent angiosome,” as it is supplied by 3 arterial avenues: (1) the first dorsal metatarsal artery arising from the dorsalis pedis artery; (2) the superficial branch of the medial plantar artery; and (3) the plantar digital arteries coming off the first plantar metatarsal artery arising from the lateral plantar artery.8
In the case of this patient, the blood supply branching off from the first dorsal metatarsal artery of the dorsalis pedis artery, as well as the superficial branch of the medial plantar artery, were heavily diseased, which resulted in poor perfusion to the vascular territory supplying the ulcerated right hallux. However, by using the angiosome concept to deliberately target these 2 avenues of blood flow and restore patency to their digital branches via endovascular therapy, we were able to successfully ensure optimal wound-healing outcomes for the patient. There is considerable evidence within the literature to further support the beneficial role of angiosome-specific revascularization in wound healing. One 2009 study, involving the analysis of 52 tibial bypass procedures performed for lower-extremity wounds, revealed that direct, angiosome-targeted revascularization produced about a 91% healing rate in comparison with a 62% healing rate for the revascularization of an artery that indirectly supplied the angiosome where the wound was present.9 In many ways, the experimental findings within this study parallel the beneficial outcomes experienced by the patient in our case report.
Conclusion
In summation, with selective imaging and proper treatment of the vessels beyond the pedal plantar loop, the arterial supply to the patient’s hallux was successfully revascularized. Although performing arterial intervention at the hallux level is quite intricate and technically demanding, for this patient, treating his disease beyond the pedal plantar loop was crucial as it allowed for good wound-healing outcomes with restoration of his balance and coordination, considering that the hallux plays a pivotal role in dynamic and static balance.10 Ultimately, through our work, we were able to improve the patient’s quality of life and prevent the threatening possibility of a costly great toe amputation.
Affiliations and Disclosures
From the 1Mayo Clinic, Scottsdale, Arizona; 2Fred Hutchinson Cancer Research Center, Seattle, Washington; 3Modern Vascular of Mesa, Mesa, Arizona; and 4AVA Vascular, LLC, Chino Hills, California.
Disclosure: The authors have completed and returned the ICMJE Form for Disclosure of Potential Conflicts of Interest. The authors report no conflicts of interest regarding the content herein.
Manuscript accepted November 15, 2021.
Address for correspondence: Grace Pyon, Mayo Clinic Arizona, 13400 East Shea Blvd, Scottsdale, AZ 85259. Email: pyon4407@gmail.com





